DIABETES
Diabetes is a well-known disease of the endocrine system. It is formally known as Diabetes Mellitus, and it is a result of the body’s inability to produce or respond to insulin, which is a hormone that allows the body to use the glucose in the food that you eat as energy, or instead store the glucose for later. Diabetes can be separated into two main types: Type 1 Diabetes Mellitus (T1DM) and Type 2 Diabetes Mellitus (T2DM).
T1DM: where the body attacks a type of its own pancreatic cells, called Pancreatic Beta Cells, and therefore these cells are not available to create insulin for the body. In this type, insulin supplementation is necessary for maintenance of proper levels of glucose, and use of glucose as an energy source in the body.
T2DM: where insulin is present, but the body is unable to respond to it properly, in turn creating an inability to use present glucose for energy. In this type, lifestyle changes in regards to diet and exercise are required to ensure glucose levels are maintained at a normal level.
Despite the substantial research behind Type 2 Diabetes, the complex mechanism by which the insulin resistance develops in the body remains unclear.
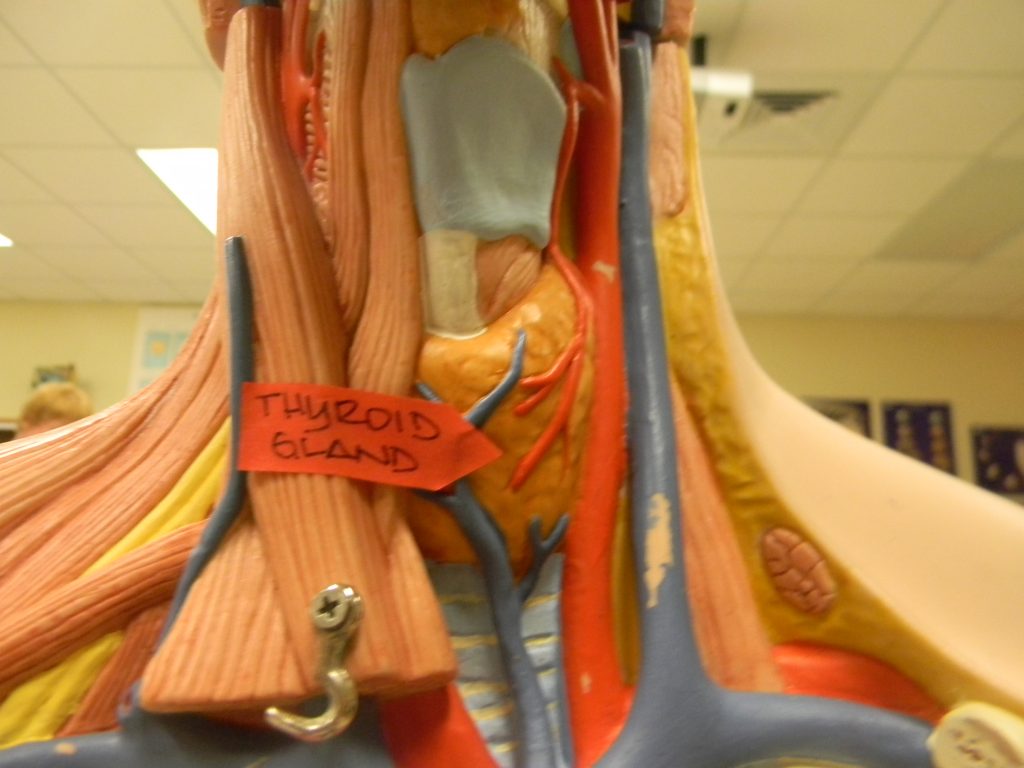
THYROID DISEASE
Thyroid disease is a potentially less familiar group of diseases of the endocrine system. The term Thyroid Disease encompasses multiple diseases that affect the thyroid gland and it’s function in hormonal regulation of the body. The thyroid gland functions to regulate the body’s metabolism- that is, the breakdown and conversion of food to energy. It does so by producing the appropriate hormones to control how fast the digestive tract, brain, heart and other parts of your body work to complete their functions.
The most common diseases of the thyroid include hypothyroidism and hyperthyroidism, however cancerous thyroid growth is also included in this category. For the purpose of this blog, we will focus on the two previously mentioned, noncancerous thyroid diseases only.
Hyperthyroidism: where the thyroid gland is overactive, creating more hormones than the body needs to regulate its metabolic functions.
Hypothyroidism: where the thyroid gland is under active, creating less hormones than the body needs to regulate its metabolic functions.
IS THERE A LINK BETWEEN DIABETES & THYROID DISEASE?
Recent research by Joffe and Distiller (2014) discusses how hypothyroidism, specifically, is associated with both T1DM and T2DM!
According to the statistics:
– The prevalence of hypothyroidism in the general population is 4%.
– The prevalence of hypothyroidism in the population of individuals with T1DM is estimated to be between 17% and 30%.
– The prevalence of hypothyroidism in the population of individuals with T2DM is estimated to be between 11% and 30%.
So why the association? Well, since the development of T1DM and T2DM have different underlying mechanisms, there are different potential reasons for the association of hypothyroidism with these separate diseases.
T1DM: Joffe and Distiller (2014) hypothesize that hypothyroidism is more greatly associated with T1DM because both diseases share a predisposition for the immune system to essentially attack itself. Specifically, for about 25% of those who are diagnosed with T1DM, unusual antibodies form in their thyroid gland that are auto reactive against thyroid peroxidase (TPOAb).
This means that these antibodies will fight and deactivate the thyroid peroxidase within the thyroid gland. Thyroid peroxidase is an enzyme that is normally present in the thyroid gland and is crucial to the production of thyroid hormone (the main hormone which regulates metabolic function). Therefore, the presence of these antibodies will create a situation where the thyroid gland appears to be “under active,” which will be diagnosed as hypothyroidism. Indeed, the authors mention that the presence of these antibodies predicts future development of hypothyroidism.
Joffe and Distiller suggest that this shared predisposition for these autoimmune diseases is most likely a result of a shared genetic predisposition. Three gene classes, CTLA-4, HLA class 11 and FOXP3, are involved in the above mechanism, and are therefore associated with risk of Type 1 diabetes as well as hypothyroidism, perhaps substantiating the link between the two.
T2DM: Unfortunately, it is mostly unclear why there is an association between type 2 diabetes and hypothyroidism. This may be related to the fact that the underlying mechanism to T2DM development is itself, still unclear. However, since hypothyroidism is seen T2DM patients in rates higher than that of the general population, Joffe and Distiller suggest multiple hypotheses to explain the association, such as:
1) Metformin: An oral diabetes medication used to control blood sugar levels in T2DM patients. Metoformin may affect an important hormone called Thyroid Stimulating Hormone, lowering it and thereby decreasing the stimulation of the thyroid gland to perform its functions.
2) Insufficient iodine intake from the diet of those attempting to control their blood glucose levels. Without iodine, necessary thyroid hormones cannot be made, and thus hypothyroidism could develop.
3) Alterations in the gut microflora (good bacteria in the digestive tract), which was found in both T2DM and thyroid dysfunction, suggesting a possible connection to hypothyroidism.
WHY IS THIS IMPORTANT?
In the case that hypothyroidism develops and remains undiagnosed in an individual with diabetes, they may suffer an increased risk of cardiovascular problems, as a result of aggravated dyslipidemia (increasing amounts of lipids like cholesterol in the blood), obesity, and vascular endothelial dysfunction. Furthermore, hypothyroidism can affect diabetes control, according to Wu (2000). It can result in increased insulin resistance and increased hypoglycemia (low blood sugar), as it is associated with impaired glucose production.
Therefore, it is important for individuals and their clinicians to be aware of the association between diabetes mellitus and thyroid disease, so that they can watch for signs and symptoms of hypothyroidism. These signs and symptoms may include, but are not limited to, fatigue, weight gain, constipation, decreased sweating, joint and muscle pains, dry skin, and slowed heart rate. The awareness of this association will aid in the recognition and ready diagnosis of hypothyroidism in individuals who are predisposed, based on their diabetes diagnosis.
With proper treatment of hypothyroidism in an individual with diabetes, cardiovascular risk can be reduced, and worsening hypoglycemia can be controlled. These important treatments will only be implemented if the individual with diabetes can recognize their symptoms, seek help and get appropriately diagnosed, therefore..
AWARENESS IS KEY!


Recent Comments